COVID-19 patients seem to behave in a somewhat unique fashion, compared to other patients with ARDS. This isn’t based on high-level data, but it seems to be a theme emerging from a variety of centers (including my experience with one patient). Some salient points are:
- Low driving pressures are seen among ventilated patients. Thus, it appears that the compliance of the lung is fairly normal (unlike most traditional ARDS patients).
- “Silent Hypoxemia” — A normal lung compliance may cause patients to have a relatively low work of breathing prior to intubation (compared to the severity of their hypoxemia).
- Highly recruitable lungs – patients often have a good response to recruitment using either high levels of PEEP or APRV (n=1 for the latter).
- Favorable response to pronation – along with the typical CT scan findings of peripheral, basilar consolidation, this might be consistent with a significant contribution from basilar atelectasis.
So COVID-19 isn’t behaving like typical ARDS, implying that it might be best treated in a slightly different manner.
Theory regarding underlying pathophysiology
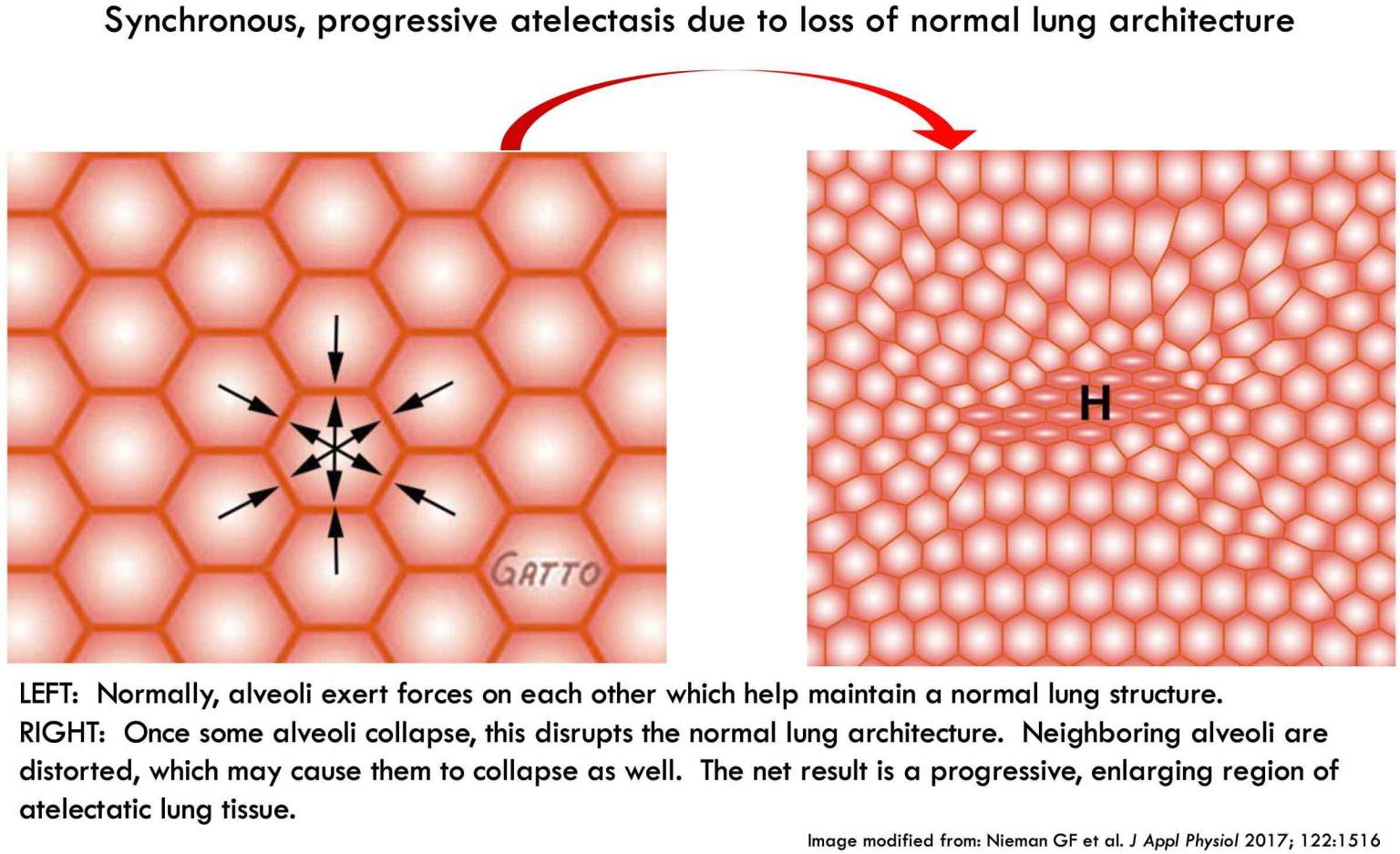 Some patients might have progressive alveolar collapse, as shown above. Alveoli start collapsing, which distorts the lung architecture and promotes collapse of neighboring alveoli. If left unchecked, this may lead to progressive deterioration which eventually requires intubation.
Some patients might have progressive alveolar collapse, as shown above. Alveoli start collapsing, which distorts the lung architecture and promotes collapse of neighboring alveoli. If left unchecked, this may lead to progressive deterioration which eventually requires intubation.
Once patients are intubated, high levels of positive airway pressure recruit the collapsed alveoli. Thus, patients may revert from a requirement for 100% FiO2 to considerably lower oxygen requirements over a period of several hours.
Best mode of noninvasive respiratory support?
The above model would suggest that COVID patients really need positive pressure more than anything else. For example, their work of breathing is often tolerable – so they may not need much mechanical support for the work of breathing (indeed, mechanical support could lead to injuriously large tidal volumes).
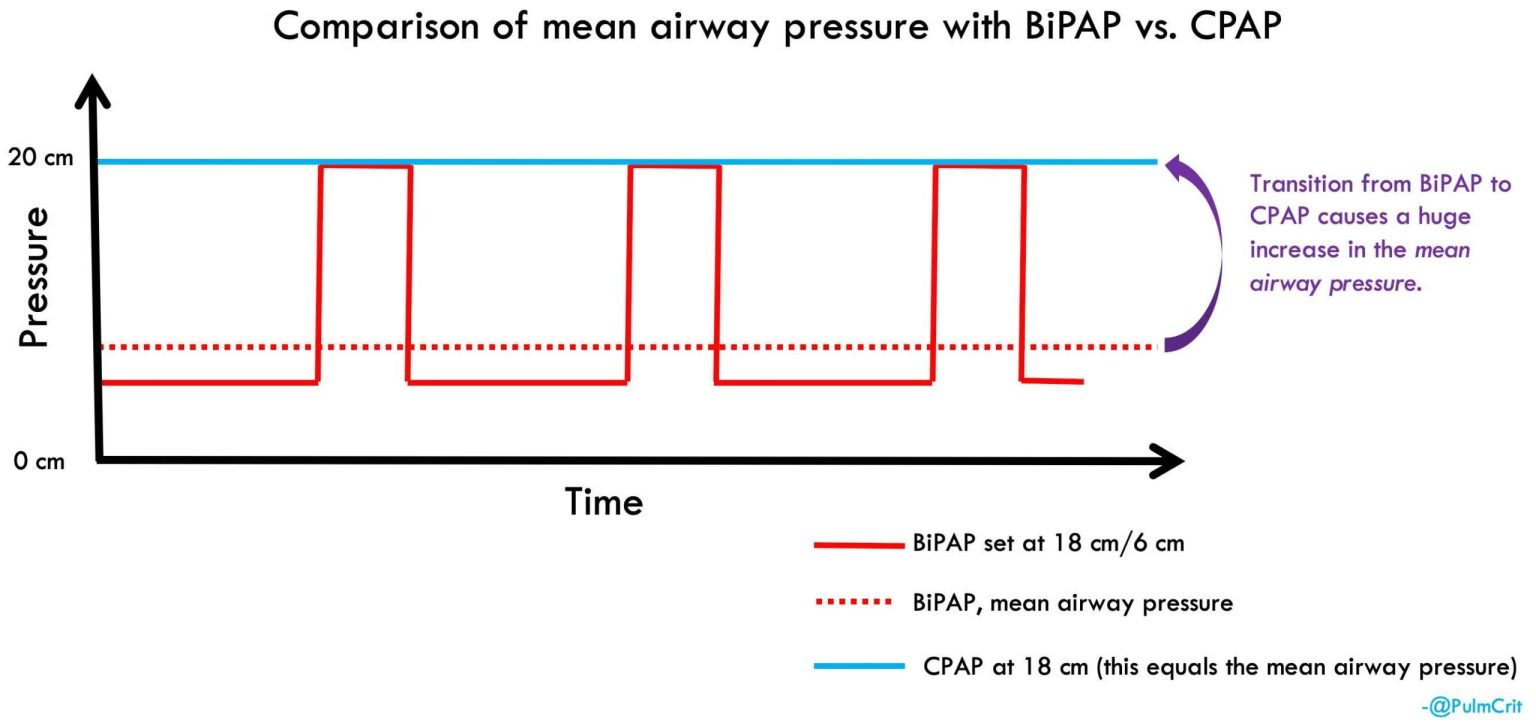
The best modality to provide lots of positive pressure is simply Continuous Positive Airway Pressure (CPAP). CPAP may not seem dramatic, but this modality actually provides the greatest amount of positive pressure to allow for the most powerful recruitment:
 CPAP may have several advantages for COVID:
CPAP may have several advantages for COVID:
- CPAP provides the maximal amount of mean airway pressure without intubation.
- CPAP doesn’t augment tidal volumes, so this may promote a more lung-protective ventilation pattern.
- With the use of a closed system and viral filters, this may be reasonably safe regarding viral transmission (nothing with COVID-19 is 100% safe).
Nuts and bolts: how CPAP might be used
- The pressure might be up-titrated as tolerated to a fairly high level (e.g. 15-18 cm). Using excessively high pressure could risk gastric insufflation and aspiration (Bouvet et al., 2014).
- The FiO2 could be titrated against patient saturation. A favorable response to CPAP would be reflected in lung recruitment and falling FiO2 requirements. Alternatively, rising FiO2 requirements would signal CPAP failure and a need to intubate.
- A helmet interface could be optimal, if available (to avoid mask seal problems).
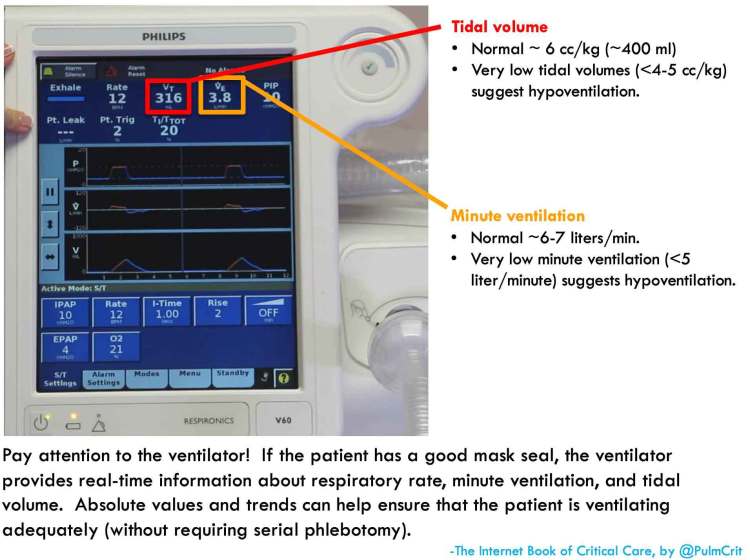
- Monitoring:
- Mental status
- Oxygenation (FiO2 requirement, oxygen saturation)
- Ventilation efficacy (tidal volume & minute ventilation on the CPAP device, perhaps intermittent VBG/ABG as clinically warranted)
What is the role of CPAP in COVID-19?
This is really unknown. There are many strong opinions, but almost no data (especially COVID-19-specific data). Unfortunately, most available evidence with regard to “noninvasive ventilation,” tends to consist largely of BiPAP (rather than CPAP). Indeed, these two modalities are invariably lumped together (despite being quite different).
CPAP certainly isn’t the treatment of choice for all COVID-19 patients. However, it could potentially play a role in certain situations:
- A patient with worsening hypoxemia (e.g. requiring ~50-60% FiO2) who is in no distress and has no other organ failures.
- Patients whose preference is to not be intubated (DNR/DNI).
- Exhaustion of the supply of mechanical ventilators (there is a large supply of CPAP machines, which are often used for obstructive sleep apnea). Similarly, if CPAP could avert intubation in even only 20-40% of patients, this could help prevent running out of ventilators.
- Lack of a team present capable of intubating the patient (e.g. a small hospital without resources necessary for immediate intubation)
As with all forms of noninvasive ventilation, careful monitoring is the key to safety. This is particularly critical for patients with COVID-19, who may develop “silent hypoxemia” (causing them to look much better than they actually are).
- COVID-19 appears to cause an unusual form of hypoxemic respiratory failure, with profound hypoxemia but normal lung compliance. This might be due to diffuse atelectasis.
- CPAP could be a desirable mode of noninvasive support for these patients. CPAP is the modality which provides the most powerful lung recruitment (highest mean airway pressure). It also has the advantage of avoiding injuriously large tidal volumes.
- The optimal role of noninvasive support modes in COVID-19 is currently unknown. CPAP could be a rational selection for some patients with moderate hypoxemia and single-organ failure. As always, further evidence is needed.
Going further
- Section on noninvasive ventilation in COVID-19 IBCC chapter.
- IBCC chapter on noninvasive respiratory support.